The Silent Killer: Sepsis and Septic Shock

Sepsis is caused by a dysregulated host response to infection, which leads to organ dysfunction. It can be life-threatening. A subset of sepsis patients develops septic shock which is defined by profound cellular abnormalities and inadequate organ perfusion. Clinical and laboratory abnormalities of the respiratory system, coagulation, liver, cardiovascular system, and kidneys are evidence of organ dysfunction. Approximately 25% of sepsis cases have detectable bacteremia. The remaining 75% have organ system infections. Sepsis can also be caused by infection with viruses, fungi, or protozoa.
Pathophysiology
The pathophysiology of sepsis involves the interaction of the host’s immune, cardiovascular, neural, metabolic, and coagulation systems with the infectious agents. Normally, some degree of inflammatory response occurs, but when this response is dysregulated, an excess of pro- and anti-inflammatory mediators, leads to organ dysfunction.
Gram-negative mechanisms: Gram-negative bacteria cause sepsis by using the endotoxin, also called lipopolysaccharide (LPS). Lipid A, the main component of LPS, binds to LPS-binding protein, and this complex interacts with the pattern recognition receptor, toll-like receptor 4 (TLR4). They are present on the surface of macrophages and other innate immune cells, as well as B cells. When macrophage TLR4 activates, it stimulates the production of interleukin-1, tumor necrosis factor, and interleukin-6. These cytokines cause fever, alter endothelial cells, leading to vascular leak, and recruit inflammatory. Vasodilation and hypotension are caused by release of nitric oxide. Endotoxin also leads to activation of the coagulation cascade, causing disseminated intravascular coagulation. The end result of this cascade is the formation of thrombi (composed of fibrin) in capillaries throughout the body, blocking blood flow and resulting in anoxia of vital organs. When blood leaks into tissue spaces at the site of endothelial cells damaged by anoxia, petechial hemorrhages and purpuric lesions occur.
Other pathogens: Gram-positive bacteria don’t contain LPS or endotoxin but contain surface components such as peptidoglycan and teichoic acid. These components bound to PRRs other than TLR4 to stimulate macrophages and to produce inflammatory mediators as mentioned above. Similarly, fungi, protozoa, and viruses that cause sepsis also trigger a similar macrophage response.
Immune & Risk Factors
Sepsis is often characterized by elevated total leukocytes count, especially neutrophils alongside a decrease in the number and function of leukocytes, especially B and T lymphocytes. This enhances the severity of infection, limits the adaptive host response, and further augments the impact of sepsis. A predisposition to sepsis occurs in very young age, very old age, people with reduced host defenses, and those with chronic diseases such as diabetes, chronic hepatitis, and kidney failure.
Neonatal sepsis: Neonatal sepsis is the result of an infant’s immature immune system coupled with the carriage of bacteria in the female genital tract that are transmitted during the passage through the birth canal.
Clinical Manifestations
The clinical manifestations include fever and elevated neutrophils, along with signs of organ dysfunction such as hypoxemia, low platelets, abnormal liver function, hypotension, mental status changes, and kidney injury.
Etiologic Agents
Sepsis is caused by a variety of pathogens:
Gram-negative bacteria
- Enterobacteriaceae (Klebsiella, Serratia, and Proteus)
- Pseudomonas
- Neisseria meningitidis
- Salmonella typhi
- Vibrio vulnificus
- Yersinia pestis
Gram-positive bacteria
- Staphylococcus aureus
- Enterococcus faecalis
- Streptococcus pneumoniae
- Streptococcus pyogenes
- Streptococcus agalactiae
- Listeria monocytogenes
- Bacillus anthracis
Viruses
- Ebola virus
- Influenza virus
- Hantavirus
- Dengue virus
- Yellow fever virus
Fungi
- Candida albicans
Protozoa
- Plasmodium falciparum
Diagnosis
For identification of the microbiological cause of sepsis, blood cultures are used to identify the microbial cause of sepsis. Other tests include urinalysis and urine cultures. Skin lesions and sputum should also be cultured.
Treatment
The treatment process includes the administration of broad-spectrum bactericidal antibiotics intravenously to cover the most likely organisms. After blood cultures are drawn, immediately start the antibiotic treatment. After the diagnosis of septic shock or sepsis are made, initiate intravenous antibiotics within the first hours. When choosing the antimicrobial drug regimen, the prevalence of antibiotic-resistant organisms should be considered.
One suggested antibiotic regimen includes vancomycin plus either a third- or fourth-generation cephalosporin or a carbapenem. An aminoglycoside or a fluoroquinolone can be added. Sepsis treatment also parallels that of the treatment of distributive hypotension shock, where intravenous fluids are used to raise blood volume. In case fluids are ineffective, hypotension can also be treated with vasopressors, such as norepinephrine. Assisted breathing using a ventilator, oxygen supplementation, and dialysis for kidney failure may be necessary. None of these will be successful without identifying and removing the original cause of infection. Generally, a foreign body such as an intravenous catheter that is infected should be removed as soon as is safely possible, and any abscess should be drained and cultured.
Prevention
The vaccines are available for N. meningitidis, S. pneumoniae, S. typhi, influenza virus, and yellow fever virus. Preventive antibiotics are given to those who develop immunosuppression and pregnant women who test positive for group B streptococcus carriage to prevent sepsis. Prompt removal of unnecessary intravenous and urinary catheters is important, as these serve as an entry point for bacteria and fungi into the bloodstream.
Epidemiology & Global Response
Sepsis is one of the main causes of morbidity and mortality in the United States. The Centers for Disease Control and Prevention (CDC) estimates that more than 1.7 million adults in America develop sepsis each year. Sepsis and septic shock cause approximately 270,000 deaths annually, with fatality rates of 30% to 50% in older patients. The conditions are estimated to cost more than 30 billion dollars each year. The incidence of infections that result in sepsis continues to rise with the increased incidence of antibiotic-resistant organisms along with increased use of immunosuppressive drugs, intravenous and urinary catheters, and prosthetic implants. To combat this important global health threat, WHO responded with a WHO secretariat report, and, in May 2017, the Seventieth World Health Assembly adopted Resolution WHA70.7 on improving the prevention, diagnosis, and clinical management of sepsis.
Similar Post You May Like
-
CFCs, HFCs and their long, troubled history
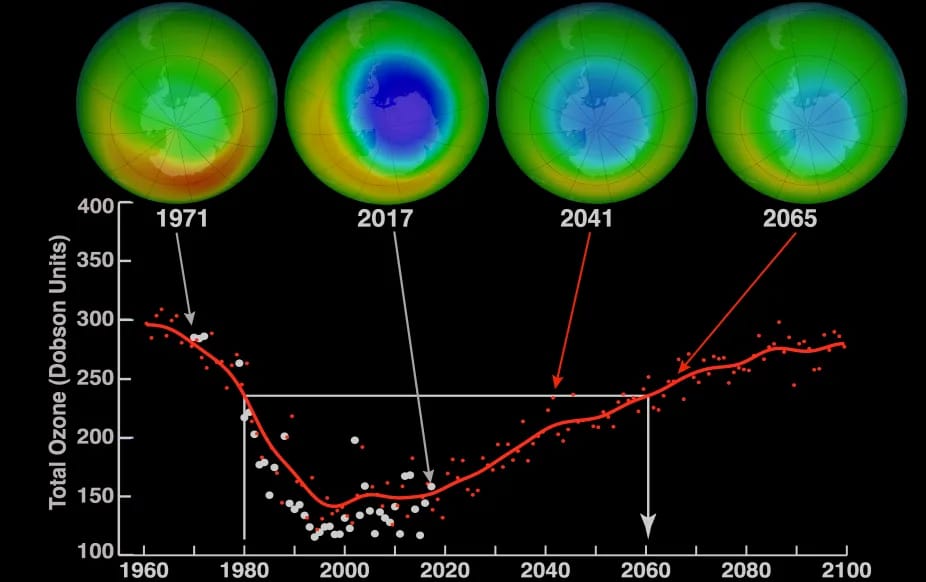
At its peak, the ozone hole covered an area 7 times larger than the size of Europe, around 29.9 million km2, and was rapidly expanding
-

The Origin of Universe: Deciding point where it all began!
Let us unravel and surf through the ideas throughout ages to understand what the universe and its origin itself was to its inhabitants across history.
-

The Artemis Program
Inspired by the Greek goddess of the Moon, twin sister to Apollo, the artimis program was named on 14 May 2019 by Jim Bridenstine.






