Mycoplasma Pneumonia: An Overview of the Bacterium and its Infections

Mycoplasmas are the smallest free-living organisms. They are 0.3 μm in diameter. Their most striking characteristic is the absence of a cell wall. They stain poorly with Gram Stain, and antibiotics that inhibit cell wall synthesis are ineffective. These organisms can exhibit a wide range of shapes because of their flexible outer surface. Its cell membrane consists of cholesterol, a sterol found commonly in eukaryotic cell membranes. They have intricate nutritional requirements, including several lipids, for growth in the laboratory on artificial media. Their growth rate is gradual, and 1 week is required by the organism to form a visible colony. The characteristics of the colony include a “fried-egg” shape, with a raised center and thinner outer edge.
Mycoplasma pneumoniae is the sole pathogen known to affect humans and causes “atypical pneumonia.” It was formerly called primary atypical pneumonia. The term atypical is applied because this type of bacterium cannot be readily isolated on routine media in a diagnostic laboratory or the disease does not resemble pneumococcal pneumonia. Atypical pneumonia is also caused by Legionella pneumophila, Chlamydia pneumoniae, Chlamydia psittaci, Coxiella burnetii, and viruses such as influenza and adenovirus.
The infections caused by M. pneumoniae occur worldwide, with increased and severe incidence in winter. The organism is the most common cause of pneumonia in young adults, and outbreaks occur in groups with close contact. It is estimated that only 10% of infected individuals get pneumonia, and it accounts for 5% to 10% of community-acquired pneumonia.
The organism is transmitted by respiratory droplets. In lungs, the organism is rod-shaped, with a tapered tip that contains specific proteins that help the organism to attach to respiratory epithelium. The organism doesn’t invade the respiratory mucosa, but it inhibits the ciliary motion, and necrosis of the epithelium occurs. The mechanism by which organisms cause inflammation is uncertain; however, it does produce hydrogen peroxide which contributes to damage in respiratory tract cells. It has only one serotype and is antigenically distinct from other species of Mycoplasma. Immunity is not complete, allowing for the possibility of subsequent episodes of the disease. However, during the infection, autoantibodies are produced against red cells (cold agglutinins) and brain, lung, and liver cells; these antibodies play a role in extrapulmonary manifestations of infection.
The onset of mycoplasma pneumonia is gradual, beginning with a nonproductive cough, sore throat, or earache. Whitish, non-bloody sputum is produced in small amounts. Constitutional symptoms of fever, headache, malaise, and myalgias are pronounced. The paucity of the findings on the chest examination is in marked contrast to the prominence of the infiltrates seen on the patient’s chest X-ray. The disease resolves spontaneously in 10–14 days. M. pneumoniae also tends to cause bronchitis.
Diagnosis is not made by culturing, since the organism takes 1 week to grow on special culture media. Culture on simple media reveals only normal flora. Currently, PCR (polymerase chain reaction) is the best diagnostic procedure. The serologic testing for antibody presence in the patient’s serum may also be useful. A cold agglutinin titer of 1:128 or higher is indicative of recent infection. Cold agglutinins are IgM autoantibodies against type O red blood cells that agglutinate these cells at 4°C but not at 37°C. However, half of the patients will be positive for cold agglutinins since the test is non-specific and false positive results occur in case of adenovirus and influenza virus infections.
The diagnosis of M. pneumoniae infections can be confirmed by a fourfold or greater rise in specific antibody titer in either a complement fixation or an enzyme-linked immunosorbent assay (ELISA) test.
The treatment of choice is either a macrolide, such as erythromycin or azithromycin, or a tetracycline, such as doxycycline. The fluoroquinolone levofloxacin is also effective. These drugs only shorten the duration of symptoms since the disease resolves spontaneously. Penicillins and cephalosporins are inactive because the organism has no cell wall. There is no vaccine or other specific preventive measure.
Similar Post You May Like
-
CFCs, HFCs and their long, troubled history
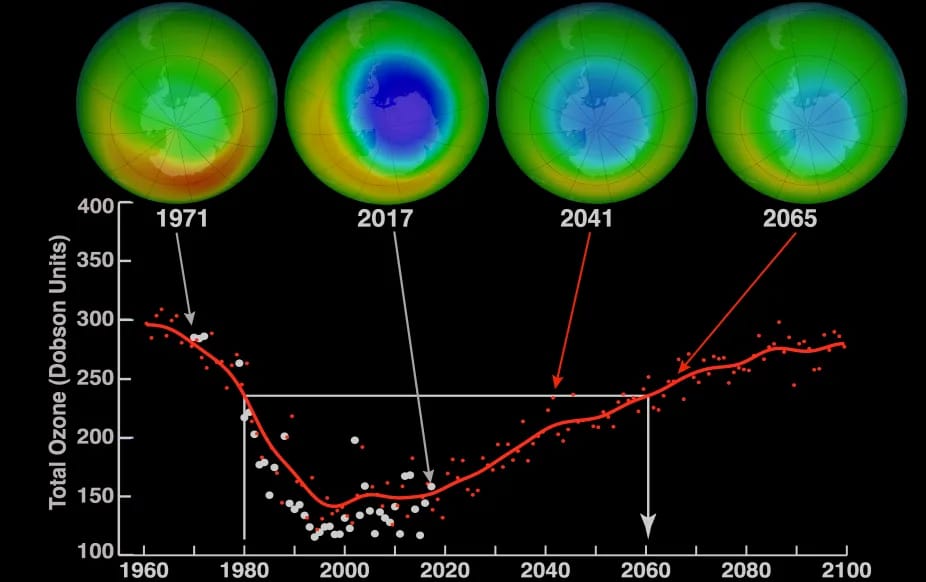
At its peak, the ozone hole covered an area 7 times larger than the size of Europe, around 29.9 million km2, and was rapidly expanding
-

The Origin of Universe: Deciding point where it all began!
Let us unravel and surf through the ideas throughout ages to understand what the universe and its origin itself was to its inhabitants across history.
-

The Artemis Program
Inspired by the Greek goddess of the Moon, twin sister to Apollo, the artimis program was named on 14 May 2019 by Jim Bridenstine.






