Brucellosis: A Zoonotic Disease with Significant Public Health Implications
.png)
Brucellae are small gram-negative rods without a capsule. Species of Brucella cause brucellosis, also known as undulant fever. The three major human pathogens are Brucella melitensis, Brucella abortus, and Brucella suis, with animal reservoirs being goats and sheep, cattle, and pigs, respectively.
These organisms are zoonotic and cause zoonoses—human diseases acquired from animals. Some zoonotic organisms are transmitted directly from the animal reservoir, while others are spread by vectors such as mosquitoes, fleas, and ticks.
In the United States, B. melitensis infections are often linked to imported cheese made from unpasteurized goat’s milk from Mexico or the Mediterranean region. The disease is rare in the U.S. because pasteurization kills the organism, but brucellosis remains a worldwide concern.
Pathogenesis
The organisms enter the body either through ingestion of contaminated milk products or via direct skin contact. They localize in the reticuloendothelial system, which includes the lymph nodes, liver, spleen, and bone marrow.
Some organisms survive within these cells, while many are killed. The host response is granulomatous, involving lymphocytes and epithelioid giant cells, which may progress to local abscess formation.
Although the exact mechanism of pathogenesis remains unclear, studies show that endotoxin plays a role in infection. No exotoxins are produced.
Clinical Features
Non-specific symptoms appear after an incubation period of one to three weeks. These include fever, chills, fatigue, malaise, anorexia, and weight loss. The onset may be acute or gradual.
The characteristic undulating (rising-and-falling) fever pattern occurs in a minority of patients. Enlargement of the spleen, lymph nodes, and liver is common. Pancytopenia—a significant reduction in red blood cells, white blood cells, and platelets—may occur.
Infections caused by B. melitensis are typically more severe and prolonged, while B. abortus infections tend to be more self-limited. Osteomyelitis, a bone infection involving the bone marrow, is the most frequent complication. Person-to-person transmission is rare.
Laboratory Diagnosis
Diagnosis is made through blood cultures or bone marrow cultures, which typically yield the organism. Recovery requires enriched culture media and incubation in 10% CO2.
A slide agglutination test can be used for rapid presumptive identification. This test involves mixing the sample with Brucella antiserum on a slide and observing visible agglutination. Species identification is confirmed using biochemical tests.
If cultures are negative, serologic testing is performed to detect a rise in antibody titer. In the absence of an acute-phase serum specimen, a convalescent-phase titer of at least 1:160 is diagnostic. PCR (polymerase chain reaction) testing is also available.
Treatment and Prevention
Doxycycline is the treatment of choice and is combined with either streptomycin or rifampin. Significant resistance to these drugs has not been reported.
Prevention strategies include pasteurization of milk, immunization of animals, and slaughter of infected livestock. There is currently no human vaccine available for brucellosis.
Similar Post You May Like
-
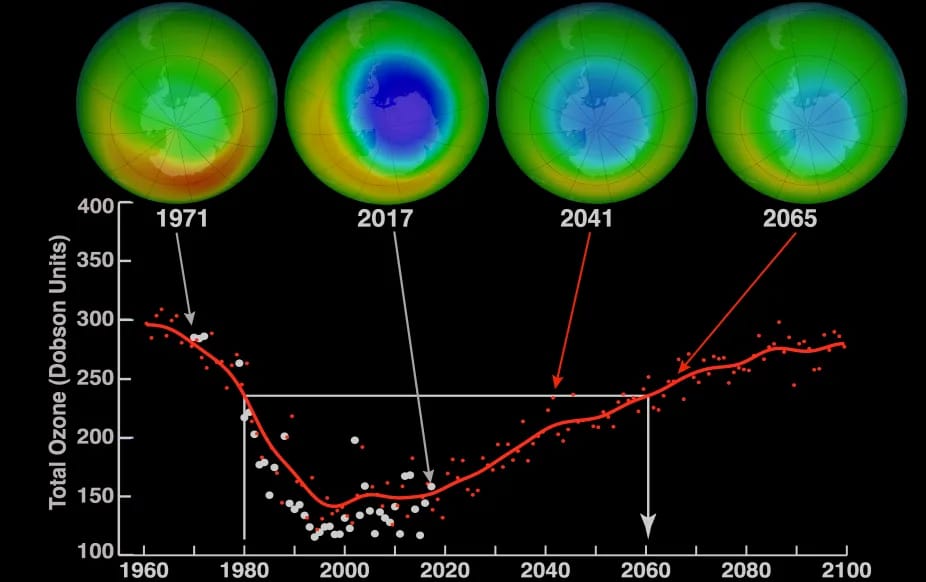
CFCs, HFCs and their long, troubled history
At its peak, the ozone hole covered an area 7 times larger than the size of Europe, around 29.9 million km2, and was rapidly expanding
-

The Origin of Universe: Deciding point where it all began!
Let us unravel and surf through the ideas throughout ages to understand what the universe and its origin itself was to its inhabitants across history.
-

The Artemis Program
Inspired by the Greek goddess of the Moon, twin sister to Apollo, the artimis program was named on 14 May 2019 by Jim Bridenstine.






